1 min read
Tennessee’s $13M Boost for Rural Healthcare
Big news for healthcare providers in Tennessee: The state is now accepting applications for the third round of...
Rather than standing up a new mobile health clinic program on your own, it may make sense to work with one of our expert program planners on proven mobile health clinic plans, policy, procedures, and even staffing.
mission, metrics & marketing
procedures, policies & people
staffing & sustainability
financial support

In late 2022, our team met with executive teams with a health system in MD and others in CA who all spoke passionately about taking care to their community with mobile clinics. They had funding, but lacked a path to power - planning, staffing, sustainability, marketing, workflow, and support services.
But I believe in the power of Team -- the right people doing the right things, at the right time and for the right reason -- and our folks stepped into the gap with them.
With a standardized model of planning, community engagement, and a blanket of best practices from mobile programs across the country, our teams have collaborated to implement effective and sustainable mobile health clinic programs.
We stand ready to help others who have identified a need, have a desire to make a difference, but are lacking planning or operational resources.


-1.png?width=1080&height=1080&name=Staffing%20(3)-1.png)
-1.png?width=1080&height=1080&name=Staffing%20(6)-1.png)
-1.png?width=1080&height=1080&name=Staffing%20(1)-1.png)
-1.png?width=1080&height=1080&name=Staffing%20(2)-1.png)
-1.png?width=1080&height=1080&name=Staffing%20(4)-1.png)
-1.png?width=1080&height=1080&name=Staffing%20(5)-1.png)
Should you tackle a new program alone?
Our collaborative model attracts diverse mobile health leaders around the country, ensuring you have access to a blanket of best practices.
For guidance, comprehensive plans for community outreach and marketing, efficient workflow and policy solutions, and detailed step-by-step workflows, partner with us. A commissioning partner is a more cost-effective and faster path to developing a sustainable program.

Partnership is a powerful strategy for health systems to improve access and outcomes PLUS expand revenue sources - with no upfront costs or capital investments. This program is a win for communities, QI teams, providers, and the C-suite.




.png?width=248&height=203&name=download%20(2).png)


.png?width=391&height=129&name=download%20(3).png)
-1.png?width=225&height=225&name=download%20(4)-1.png)

.png?width=233&height=88&name=logo%20(3).png)
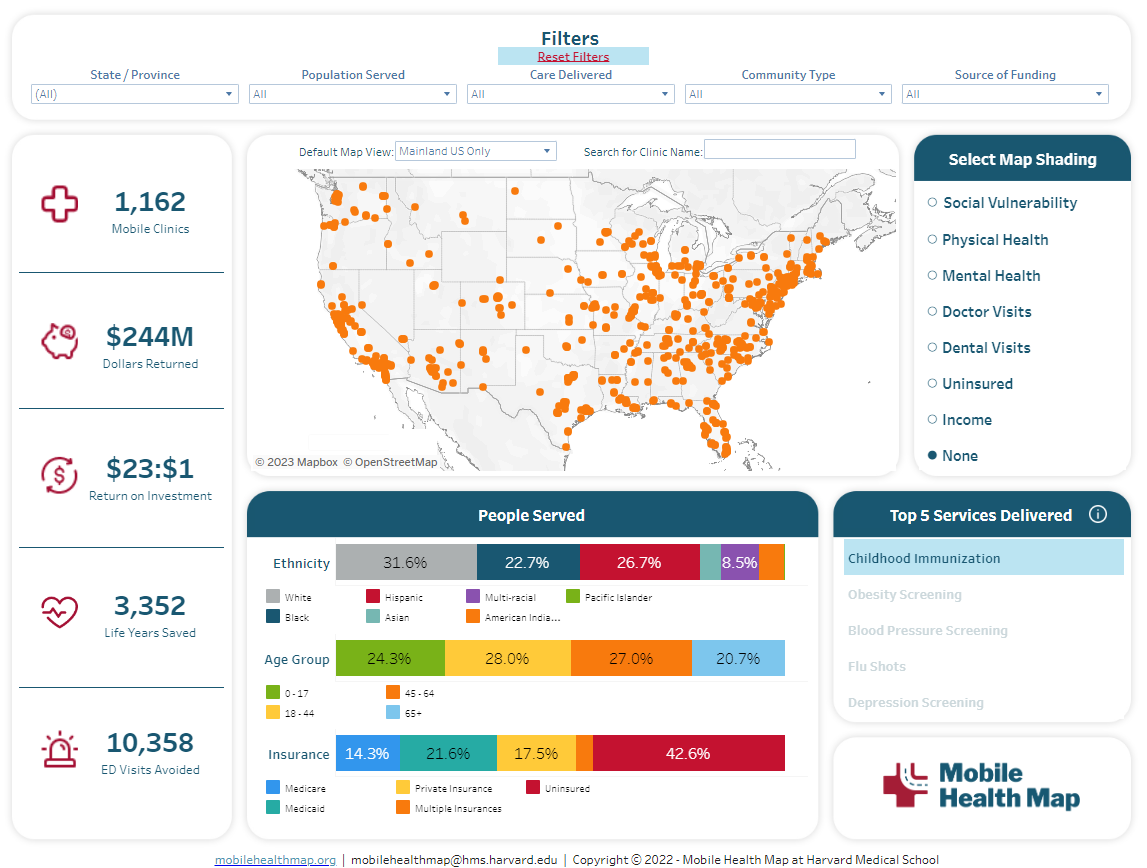
Fostering health equity begins with understanding where, exactly, the care gaps lie.
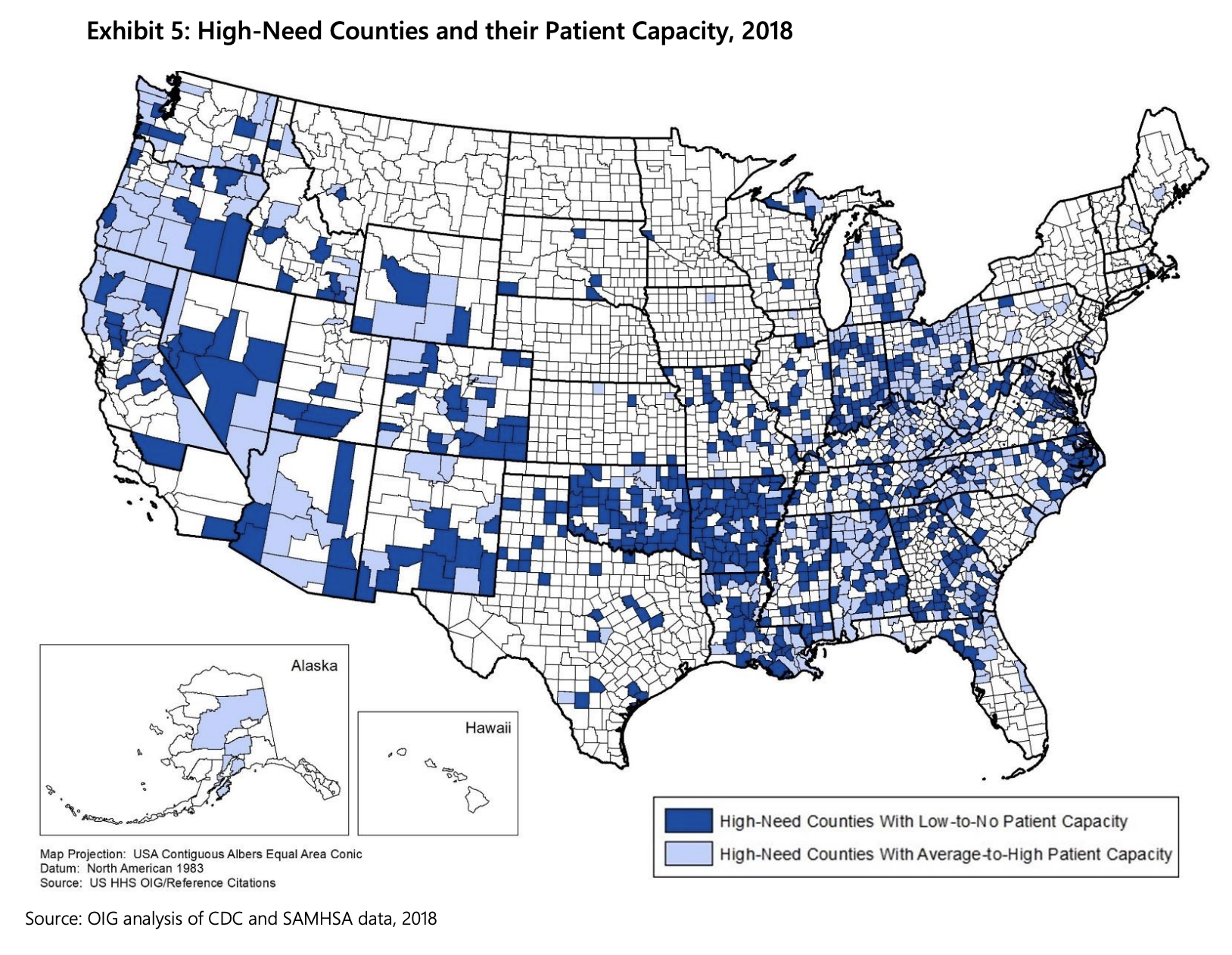
For example, when availability of buprenorphine services are mapped, 40% of counties have 0 waivered providers. Depicted in this report from OIG, "a swath of the United States from the Upper Midwest region and Great Plains to Texas and the Southeast have large areas of low to no capacity to provide buprenorphine services."
Correlated with the 381 US counties with the highest indicators of opioid misuse and abuse counties, you find areas likely to be facing the most critical need for treatment services (12 percent of all counties nation-wide). 62% of these highest-need counties are in rural areas.
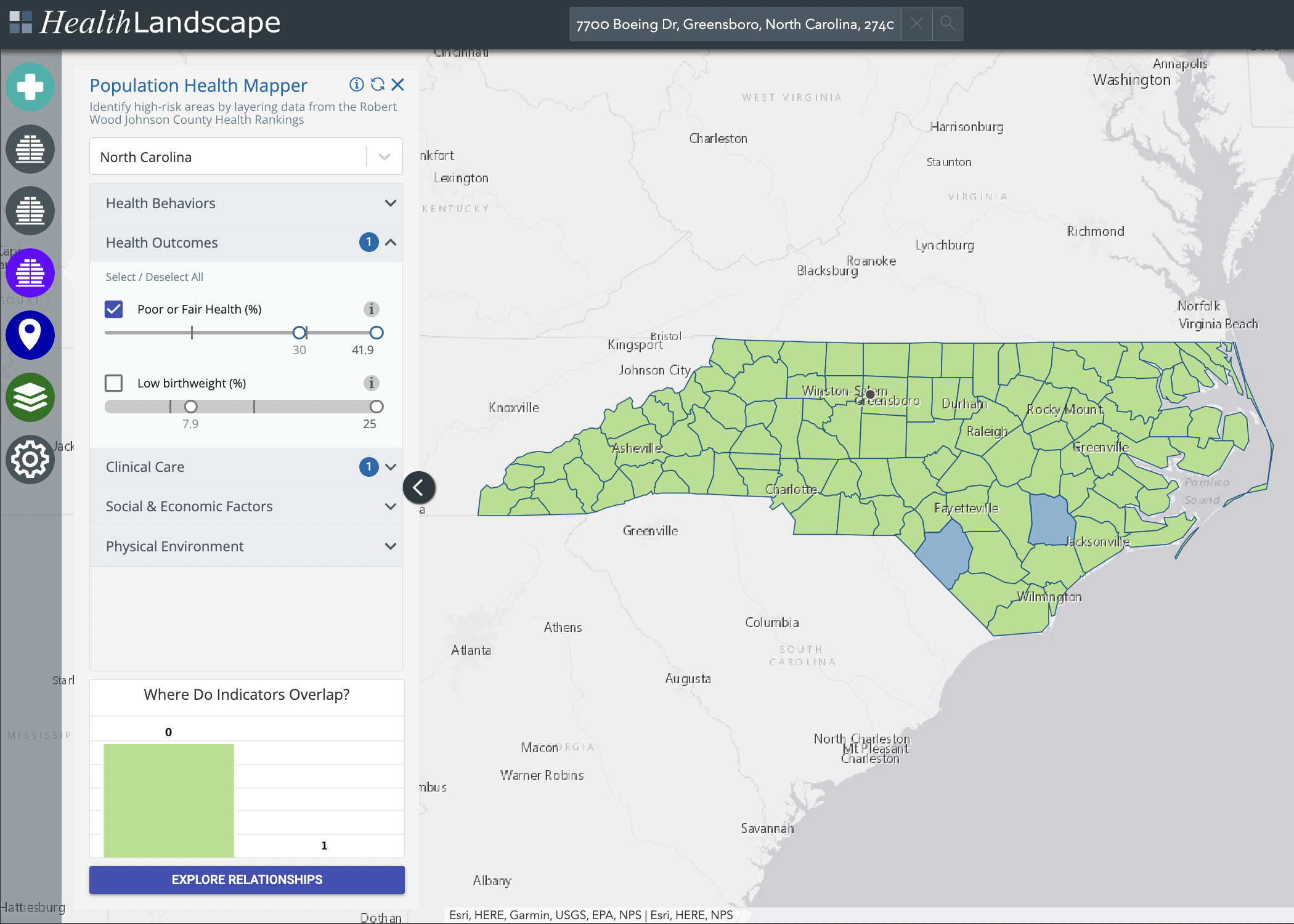
When State agencies provide funding or focus to help local providers deploy a mobile health clinic, we use UDS or GIS data to find the people that need them most.
For this example, NC UDS data shows two counties have healthcare complexity - poor health outcomes and a high population of uninsured.
At a high level, targeted deployment of mobile outreach, education or primary care efforts will improve outcomes and reduce Payer spending with minimal investment or risk.
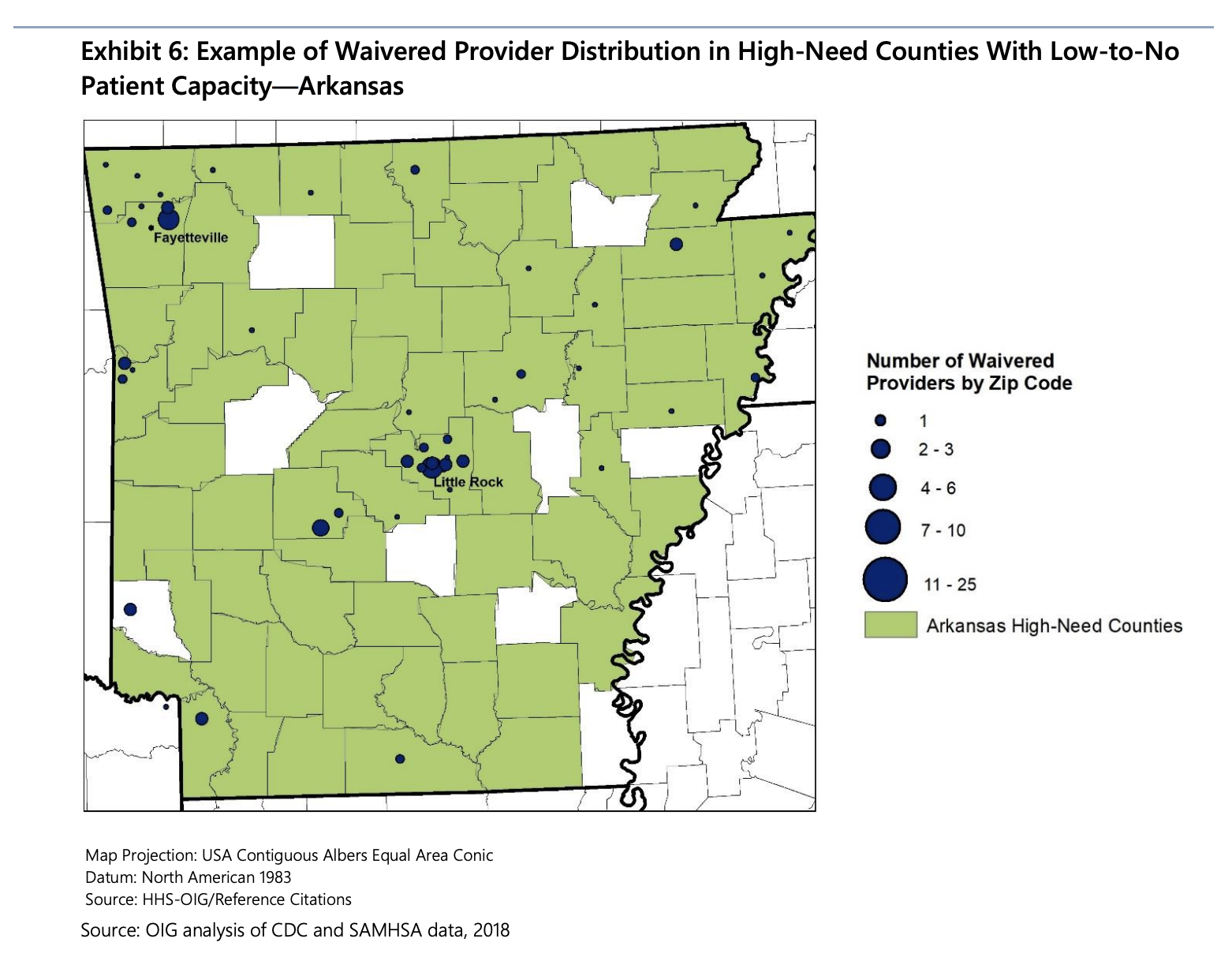
From the same data set, two high-need counties in Arizona can be highlighted. Notice nearly all waivered providers were driven by economic incentives to locate offices near the major population centers of Phoenix and Tuscon. Persons living and working in the same county may still not have adequate access to waivered providers.
For example, individuals with SUD residing in southwest Maricopa County would have to drive an estimated 115 miles (2 hours) to access buprenorphine services in the Phoenix area. This same individual would have the same access issues if attempting to see a waivered provider in neighboring counties.
Deploying an SUD-oriented mobile clinic in this county to provide outreach, education, and navigation services would be recommended.
by Mission Mobile Medical
Big news for healthcare providers in Tennessee: The state is now accepting applications for the third round of...
by Mission Mobile Medical
The Mother Cabrini Health Foundation is now accepting letters of intent (LOIs) for its 2025 grants program, aimed at...
by Mission Mobile Medical
The Florida Blue Foundation is now accepting applications for its 2025 Mental Well-Being Grant Program, aimed at...
“The behind-the-scenes work you guys are doing saves lives. So thank you, every step of the way, for everything every one of you does."
-2.jpg)